We Believe in Breast Health Education
A CASE FOR SUPPORTa timeline oF our disconnect
Historically, medical guidelines encouraged women to be educated on Breast Self Exams (BSE) starting in high school.
2002
The “Shanghai Study” revolutionized breast health by finding that the teaching of BSE was unlikely to reduce mortality from breast cancer. Yet in the author’s own words,
“This was a trial of the teaching of BSE, not of the practice of BSE. It should not be inferred from the results of this study that there would be no reduction in risk of dying from breast cancer if women practiced BSE competently and frequently.”
- D Thomas, et al. p.1456
Over the next 15 years, medical guidelines backed away from teaching BSE. A campaign for “breast awareness” filled its place.
2003
American Cancer Society (ACS) states BSE are optional, “Women should be familiar with how their breasts normally look and feel and should report any changes to a health care provider right away.”
2009
United States Preventative Services Taskforce (USPSTF) “recommends against clinicians teaching women how to perform breast self-examination. (Grade D recommendation)”.
2017
American College of Obstetricians & Gynecologists (ACOG) issues bulletin, “BSE is not recommended in average-risk women because there is a risk of harm from false-positive test results and a lack of evidence of benefit.”

“Women should be educated about the signs and symptoms of breast cancer and advised to notify their health care provider if they notice a change such as pain, a mass, new onset of nipple discharge, or redness in their breasts.”
- ACOG 2017 bulletin
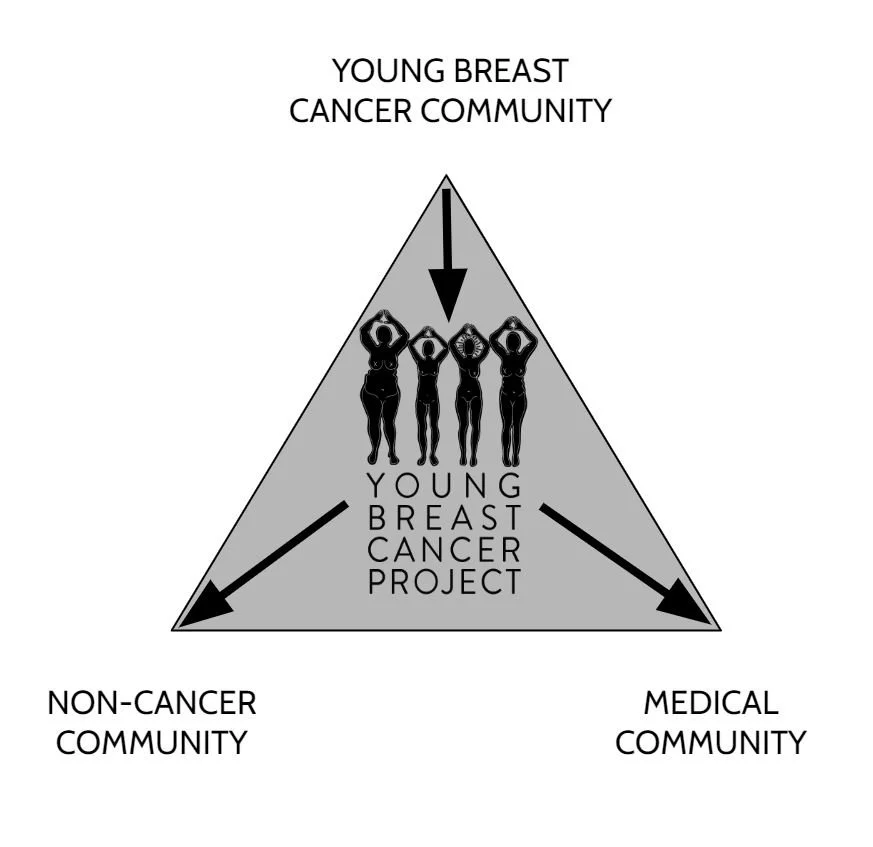
why we’re here
Our RESEARCH found that 62% of YOUNG SURVIVORS DID NOT FEEL THEY WERE EDUCATED on BREAST HEALTH by a PHYSICIAN PRIOR to DIAGNOSIS.
Without proper education, many women do not know to advocate for themselves, especially if informed they're 'too young’.
The average adolescent and young adult (AYA) breast cancer patient is diagnosed at a higher stage and has a higher mortality rate compared to their 40+ counterparts.
Mortality rates are even higher amongst young BIPOC persons and non-binary folks.
Average Risk Young women are too young for MAMMOGRAMS, and must rely on self-detection.
This affects more than young women. The American Cancer Society recommends that women of average risk begin annual mammograms at 45 (with the option to start at 40). As of 2024, the U.S. Preventive Services Task Force (USPSTF) has changed their guidelines to recommend mammograms every other year starting at age 40 rather than 50, which was their prior recommendation. The American College of Obstetricians and Gynecologists (ACOG) continues to recommend that mammograms be offered starting at age 40.
Many YOUNG women are turned away by their physicians, told they’re ‘Too Young’ or ‘NOT HIGH RISK’, causing delays in Diagnosis.
Nearly 50% of our survey participants experienced delayed diagnoses due to a medical provider’s failure to order imaging or biopsies after evaluation.

ADA, 38, ignored symptoms for 3 years. Ada was diagnosed with Stage IV de novo.

NIYA, delayed 5 months. She was breastfeeding and assumed the lump was a clogged duct.

STEPHANIE, 30, delayed 7 months. She was offered psych meds & eval because she returned 3x about a breast lump.

PATRICIA, 27, delayed 10 mths. OB/GYN was reassured by the lump feeling tender and didn't order diagnostics.

CHIARA, 27, was sent home from radiology reassured she was "too young, it's just a cyst". A year later she was diagnosed with Stage IV de novo.

ALEXIS, 29, delayed 18 months. Docs incorrectly reassured her the lump was a "benign fibroadenoma".

MISSY, 34, delayed 11 months. Her radiologist incorrectly reassured her it was a "benign fibroadenoma".

DI, 36, delayed 2 mths. Di was diagnosed with mastitis when she had Inflammatory Breast Cancer, Stage IV de novo.

MARICIA, 36, delayed 7 months. OB/GYN incorrectly reassured her the nipple crust was "dermatitis".

MIROSLAVA, 27, delayed 10 months. Miros had an aching breast and was reassured it was "nothing".

SHONTE, 25, had a leaky nipple for 2 years and was told it was a hyperactive duct. She was then diagnosed Stage IV de novo.

ANDI, at 16 years old she hid her symptoms of Inflammatory Breast Cancer until it was too late, diagnosed Stage IV de novo.

MELISSA, 34, delayed 7 months. She waited to see a physician because her mother had a history of breast cysts.